In Focus delivers deeper coverage of the political, cultural, and ideological issues shaping America. Published daily by senior writers and experts, these in-depth pieces go beyond the headlines to give readers the full picture. You can find our full list of In Focus pieces here.
The three medical personnel who run the clinic, one gynecologist and two nurses, offer a specific form of medicine to their patients struggling with infertility that is becoming increasingly popular among conservative circles, including President Donald Trump’s domestic policy advisers.
Republicans and conservative organizations have become more aware of restorative reproductive medicine, or RRM, following the upheaval over in vitro fertilization policy that started in the spring of 2024.
In the aftermath of the Supreme Court’s decision to overturn Roe v. Wade in 2022, the legal status of embryos created via IVF has loomed as a question over the GOP.
On the campaign trail last year, Trump called himself the “father of IVF” and promised to make in vitro fertilization and other assisted reproductive technologies covered benefits under Obamacare. That move alienated social conservatives and anti-abortion advocates within the Republican base, who oppose the destruction of embryos involved in the standard methods of IVF practice in the United States.
In February, Trump issued an executive order directing the Domestic Policy Council to explore policy solutions to make IVF more affordable, including an insurance coverage mandate. Since then, conservative advocacy groups have increasingly pushed RRM as a more natural, more ethical, and less costly policy alternative.
Since Trump’s executive order, conservative groups and anti-abortion advocates have spoken with White House staff in attempts to include RRM in the Trump administration’s plans for fertility policy.
RRM has also been billed by conservative groups as complementary to Health and Human Services Secretary Robert F. Kennedy Jr.’s Make America Healthy Again movement because of its emphasis on root causes of infertility as a symptom of a chronic condition, rather than on surgical or pharmaceutical treatments.
The International Institute for Restorative Reproductive Medicine is holding a briefing on Tuesday with various policy staffers on Capitol Hill to promote RRM techniques for treating infertility.
Many RRM techniques, such as diet and lifestyle changes or endometriosis surgery, can be and increasingly are incorporated into secular medical practices.
But certain Catholic medical professionals, including those at the Gianna Center, have been practicing a particular form of RRM called natural procreative technology, or NaPro, for decades to help patients either prevent pregnancy or get pregnant within the ethical guidelines of the church.
Catholic restorative reproductive medicine
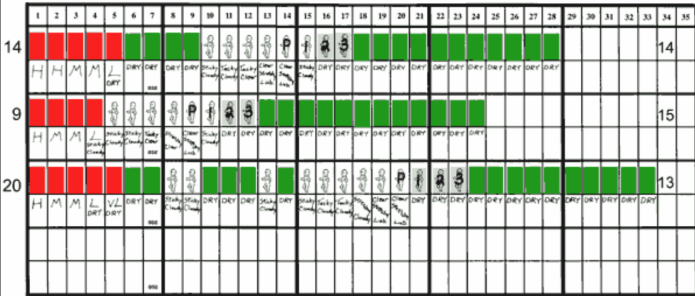
NaPro was developed by Catholic physician Thomas Hilgers in the late 1980s and early 1990s. At the core of the method is the Creighton Model of cervical mucus charting and recording of other menstrual cycle indicators.
The Creighton Model was developed based on a study funded by the National Institutes of Health to track over 4,000 ovulation cycles. That study led to the creation of a standardized system that allows women to chart their biomarkers to determine their fertility windows and possible underlying health conditions.
Licensed OB-GYNs and other medical professionals can become certified in NaPro at the Saint Paul IV Institute in Omaha, Nebraska, established by Hilgers and named after the Roman Catholic pope who prohibited the use of hormonal contraception in 1969.
Medical professionals trained in NaPro are able to use a combination of cervical mucus data, hormone levels, and other inputs to treat a variety of conditions, ranging from infertility and repetitive miscarriage to postpartum depression and premenstrual syndrome.
The most common NaPro treatments for infertility involve exploratory laparoscopic surgery to remove endometriosis, or tissue that is similar to the uterine lining that grows outside of the uterus and can cause painful periods.
NaPro surgical techniques involve removing the roots of endometriosis tissue, whereas more mainstream endometriosis surgery uses ablation, which essentially burns the tissue and can leave scarring.
Theresa Strenge, a registered nurse and volunteer at the Gianna Center, told the Washington Examiner that she started as a patient and that her seventh child is a “NaPro baby.”
Strenge said she did not need surgery but rather progesterone treatment, a hormone essential for maintaining pregnancy and another go-to tool in NaPro.
Barbara Rose, the head nurse practitioner at the Gianna Center, treated Strenge using the Creighton Model cycle chart. Strenge told the Washington Examiner that, when she told Rose about two days of brown bleeding at the end of her menstrual cycle, Rose said it could be a sign of low progesterone, a hormone essential for maintaining pregnancy.
“In that very cycle, I achieved pregnancy and I miscarried, and it was like an anvil fell on my head,” Strenge told the Washington Examiner. “I thought, ‘They really know what they’re talking about. She practically predicted this.’”
Strenge said she believes NaPro is “women’s healthcare par excellence, bar none.”
“Women, they’ve been underserved, and we don’t even realize it. We just accept it,” Strenge said, referring to the mainstream practice of using hormonal contraceptives to treat various women’s health conditions.
Inside the Catholic clinic
The Catholic identity of the Gianna Center is unmistakable despite its unassuming location in a medical office park at a busy intersection in Norristown, Pennsylvania.
In the front of the small office, the Bible verse Proverbs 31:25, about women’s “strength and dignity,” hangs on the wall. Several statues of the Virgin Mary and a portrait of Saint Paul VI populate the office, alongside a mix of religious and feminine imagery.
The practice, and several others like it across the northeast, takes its name from St. Gianna Beretta Molla, an Italian pediatrician who chose not to abort her fourth child despite developing benign tumors on her uterus during her pregnancy in the 1960s. She died roughly a week after successfully delivering her daughter and was canonized in 2004.
Rose said an average of 25 women a month call to ask to become new patients at the clinic, all based on word of mouth.
Because the Gianna Center is a nonprofit medical organization, it is able to treat any patient regardless of insurance type, including Medicaid patients.
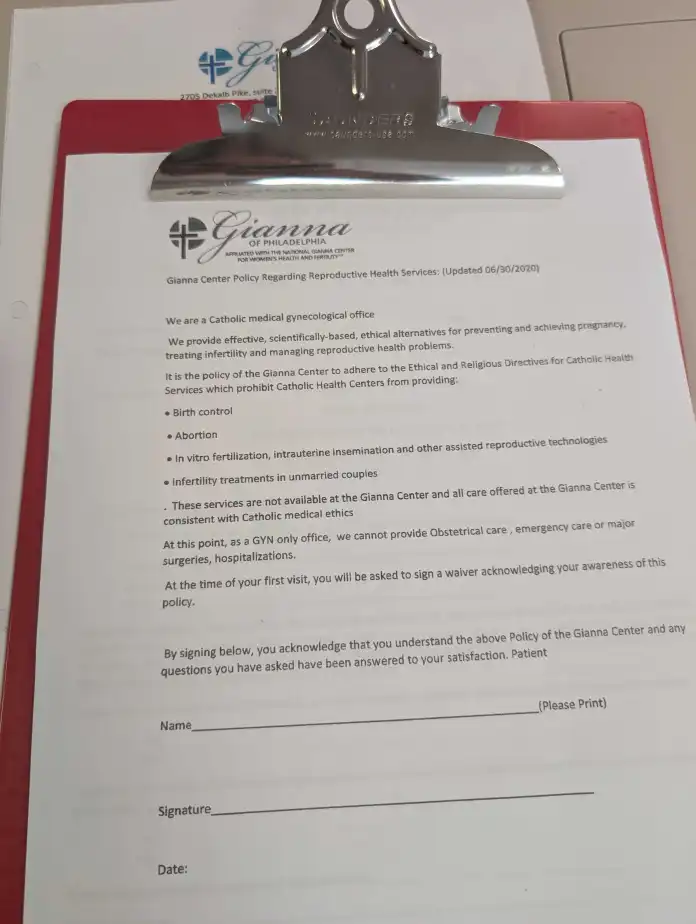
But the Gianna Center follows the Ethical and Religious Directives for Catholic Health Care Services set by the Roman Catholic Church, meaning that it will only provide NaPro fertility care to married couples looking to conceive.
“We’re a nonprofit, and because we don’t pay taxes and we’re identified by the state of Pennsylvania as a religious nonprofit, they can’t sue us for not doing these things,” Rose said. “It’s part of our religious rights. So this is how we operate.”
Intake paperwork for the Gianna Center informs patients that the clinic does not provide birth control, abortion, IVF, or other assisted reproductive technologies, or “infertility treatments in unmarried couples.”
Rose also told the Washington Examiner that healthcare professionals seeking to train at the Saint Paul VI Institute in Omaha must commit to following the Ethical and Religious Directives of the church in order to become a certified NaPro specialist, but anyone is able to audit the course.
The criticism: An ‘unmedical approach’ to fertility
The American College of Obstetricians and Gynecologists, in its issue brief on RRM, calls it an “unmedical approach” to fertility care, saying that it limits patients’ access to interventions and delays time to pregnancy.
According to the ACOG’s policy brief, because RRM is typically associated with religious practices, it excludes gay and lesbian couples and solo parents.
“Proponents of RRM advocate for policies that encourage a nonmedical and nonpatient-centered approach, discourage medical interventions, and establish barriers to evidence-based fertility care, thereby jeopardizing people’s ability to start and grow their families,” according to the ACOG.
An ACOG spokesperson declined the Washington Examiner’s request for an interview on RRM and NaPro.
Dr. Kaylen Silverberg, an IVF specialist with the Texas Fertility Center and medical adviser to the lobbying group Americans for IVF, told the Washington Examiner that he does not have a problem with RRM in and of itself, but rather with any insistence that RRM is the only option for couples.
He equated RRM to recommending diet and exercise changes for a patient actively having a heart attack instead of using the most up-to-date medical science to stop the patient’s pain.
“In no field of medicine would anybody think that’s acceptable, except infertility,” Silverberg said. “These people are actually making an argument that restorative reproductive medicine should be enough, and if you just do that and everything will be fine.”
Success of IVF versus NaPro
One in five heterosexual married couples in the U.S. struggles with infertility, or not being able to get pregnant after one year of trying, according to the Centers for Disease Control and Prevention.
Silverberg, who has practiced reproductive medicine for more than 30 years, said there is only about a 15% chance in a given menstrual cycle that a healthy couple will conceive and carry a baby to term naturally, even without diagnosed infertility.
Most fertilization events, where egg meets sperm, result in miscarriage without women even knowing it, he says, usually because of embryonic genetic abnormalities incompatible with life.
“In nature, those embryos die, and a woman has a period,” Silverberg said. “She never knew whether she even got a fertilized egg or not. She just knows that she didn’t get pregnant. She has a period.”
Neither IVF nor NaPro is guaranteed to produce a healthy pregnancy.
According to the Society for Assisted Reproductive Technology, the success rate for IVF for women under 35 was more than 51% in 2022. That drops off to about 38% for women between the ages of 35 and 37, and 25% for women up to 40.
Because of all the personal factors that can affect the success of IVF, such as age, weight, prior pregnancies, and other health conditions, the CDC has an IVF success calculator tool rather than providing generic approximations.
Data comparing NaPro to IVF are scant, in part because NaPro is still outside the mainstream. But some studies suggest that they have comparable results if practiced well.
A 2013 article in the American Medical Association Journal of Ethics summarizing the literature on IVF and NaPro comparisons found that achieving live birth through NaPro “may take longer,” but “it has a greater chance of occurring than with IVF.”
More recently, a report this year from the Ethics and Public Policy Center, an anti-abortion research organization, found that NaPro and other RRM techniques have success rates “similar to or better than IVF for many couples.”
RRM versus IVF: Patient experience
Shelby Kearns, a development coordinator for a domestic violence center in Florida, told the Washington Examiner that she has been treated at both a traditional fertility clinic and by NaPro specialists. From her experience, she sees the two as mutually exclusive because of how they approach the problem of infertility.
“I don’t think they can coexist because infertility is a symptom, rather than itself a disease,” Kearns said. “IVF doesn’t treat infertility like a symptom of an underlying disease. It’s just trying to treat the condition of ‘I’m not pregnant right now, and I want to be.’”
Kearns wrote in an opinion piece for the Freeman that she underwent six failed intrauterine inseminations, or IUI, during her fertility journey at an Oklahoma fertility center before moving to Florida. She wrote that she felt her clinic was “fast-tracking [her] towards IVF,” which she described as a “non-option” because of her ethical convictions.
Kearns told the Washington Examiner that she spent significantly more time per session with her Creighton Model coach and her NaPro physician than with the team at her former mainstream fertility clinic. She says that having that extra time, compared to being rushed in a traditional medical office setting, helped her get holistic treatment for underlying conditions.
“It turns out, with a little more time and with a method like NaPro, a woman or a man, for that matter, can get the diagnosis that they need,” Kearns said.
Kearns said she has just finished the three-month recovery window from her laparoscopic surgery to remove endometriosis and is starting her first cycle of trying to conceive with her husband.
Even after using NaPro to get to the bottom of chronic health problems, however, some women still struggle to get pregnant and to carry to term.
RRM, MAHA, and the IVF coverage mandate
NaPro, which is only a small subsection of the broader RRM umbrella, could not be combined with IVF because it follows the ethical guidelines of the Roman Catholic Church, which is opposed to assisted reproductive technologies.
But conservative groups have argued that other RRM techniques, ranging from surgery to remove endometriosis tissue or lifestyle-related changes, can be integrated into mainstream infertility treatment and ought to be taken more seriously.
Emma Waters, a policy analyst on biotechnology and reproductive medicine for the Heritage Foundation, told the Washington Examiner that she frames the debate as RRM working hand in hand with IVF and other assisted reproductive technologies, with the former treating the root causes of infertility and the latter being the last resort.
Waters cited a study in which couples who initially pursued RRM and then chose to pursue IVF had higher success rates than those who jumped straight into the mainstream treatments for infertility.
“Restorative reproductive medicine works prior to or alongside IVF or other approaches to treating infertility,” Waters said, adding that there is “a lot more that we can do to set couples up for success here in a way that actually boosts their overall success rates.”
Noah Brandt, the vice president of communications for the anti-abortion group Live Action, told the Washington Examiner in June that RRM is “as MAHA as it gets” because of its emphasis on root causes. Live Action presented a memorandum to the Domestic Policy Council, obtained by the Washington Examiner, that painted RRM as the MAHA alternative to IVF.
The Washington Examiner made multiple attempts to contact members of the Domestic Policy Council regarding the role that RRM might play in the IVF guidance promised by the administration this spring.
BREASTFEEDING, SUNSCREEN, AND OTHER OVERLOOKED ITEMS IN MAHA REPORT
In June, White House spokesman Kush Desai said the council “worked closely with external stakeholder groups for nearly three months” to craft the policy guidance on IVF access, but he did not elaborate on the timing of when that guidance would be made public.
The White House declined the Washington Examiner’s request for an update.















